Exploring the Diverse Landscape of Healthcare Systems Across Europe
When we think about well-being and the frameworks that support it, it’s fascinating to see the variety of models that exist. From comprehensive public programs to innovative private initiatives, many approaches aim to ensure that everyone receives the care they need. This diversity reflects not just different historical contexts, but also varying cultural values that influence how services are delivered and perceived.
Exploring these frameworks allows us to understand how different regions tackle common challenges like accessibility, efficiency, and quality of care. While some areas prioritize universal coverage, others may focus on enhancing competition among providers. This interplay creates a rich tapestry of practices that can inspire new ideas and solutions.
Moreover, numerous factors–such as demographics, economic conditions, and policy decisions–play significant roles in shaping how these organizations operate. By examining these influences, we can gain insights into what works well, what doesn’t, and where improvements could be made. Join us as we delve into the intricate world of health services provision across the continent, uncovering both successes and areas for growth.
Comparative Analysis of European Health Models
When we delve into the various frameworks for healthcare provision across the continent, we uncover a rich tapestry of approaches and philosophies. Each nation has crafted its own unique method of delivering care, influenced by historical, cultural, and social factors. By examining these diverse practices, we can gain valuable insights into what works, what doesn’t, and why these differences matter.
One major distinction lies in how services are funded and the level of access provided to individuals. Some countries prioritize universal access, ensuring that basic care is available to all, while others may adopt a more market-oriented approach, where private entities play a significant role. This can lead to disparities in both quality and availability of treatments.
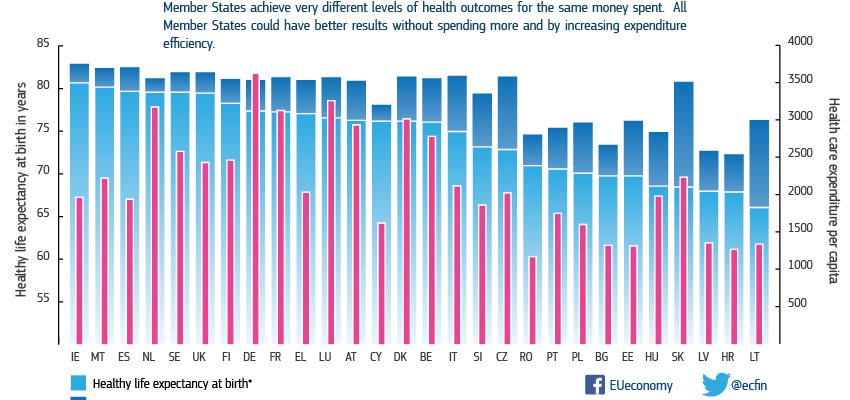
Additionally, the efficiency of management and the allocation of resources can vary widely. Some nations excel at integrating technology and innovative practices, which can streamline processes and enhance patient experiences. Conversely, others may struggle with bureaucratic challenges that impede swift decision-making and responsiveness to patient needs.
Lastly, the cultural attitude towards wellness and preventative measures can shape how communities engage with their providers. In some areas, a proactive approach to health–emphasizing prevention and early intervention–can drastically improve overall outcomes, while in regions where reactionary care dominates, chronic diseases can flourish.
By analyzing these varied methodologies, we not only learn about the multiple paths to achieving optimal care but also identify potential lessons and best practices that could benefit others. Ultimately, understanding these differences can guide future policies and reforms aimed at enhancing the overall well-being of populations.
Challenges Facing Healthcare Accessibility
Accessing medical services remains a significant hurdle for many individuals. Various factors contribute to this reality, making it difficult for people to receive the care they need in a timely manner. It’s crucial to understand the underlying issues that create these barriers and how they affect overall well-being.
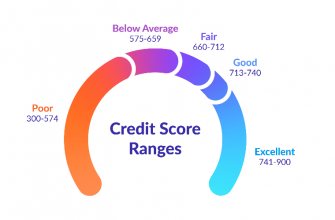
Financial Constraints: One of the most pressing obstacles is the cost associated with medical treatment. For many, exorbitant fees can deter them from seeking necessary assistance. Even those with insurance may face high deductibles or co-pays, leaving them feeling vulnerable when health concerns arise.
Geographical Disparities: Location plays a vital role in accessibility. Urban areas typically boast more facilities and specialists, while rural regions often struggle with insufficient resources. This imbalance can lead to long travel times for patients in need of specialized care.
Language Barriers: Communication is key in receiving proper treatment. For individuals who are not fluent in the dominant language, misunderstandings can occur. This can prevent patients from fully conveying their needs or understanding medical advice, leading to poor outcomes.
Workplace Policies: Many people find it challenging to balance their jobs with the need to access medical assistance. Unsuitable work schedules and lack of support from employers can discourage individuals from prioritizing their health. This situation often forces individuals to choose between their job and seeking treatment, creating additional stress.
Lack of Awareness: Education about available services is crucial. Many individuals remain unaware of the options accessible to them or how to navigate the complexities involved in getting help. This ignorance can prolong suffering and exacerbate health issues that could have been easily managed.
Addressing these challenges requires concerted efforts from policymakers, communities, and healthcare providers. By understanding the multifaceted nature of accessibility issues, we can work towards a more equitable approach that ensures everyone receives the care they deserve.
Innovations in European Medical Practices
In recent years, the realm of medical care has witnessed a remarkable transformation, driven by groundbreaking advancements and creative approaches. Across the continent, practitioners and researchers are embracing new technologies and methodologies that challenge traditional norms. This shift not only aims to enhance the quality of treatment but also seeks to empower patients through personalized solutions and innovative practices.
Telemedicine has emerged as a game-changer, enabling virtual consultations that break geographical barriers. Patients can now connect with specialists from the comfort of their homes, ensuring timely access to expertise. This approach has proven particularly beneficial in rural areas, where medical resources may be scarce.
Another exciting development is the integration of artificial intelligence in diagnostics. Cutting-edge algorithms can analyze medical data more efficiently than ever, assisting professionals in identifying patterns and making informed decisions. This technology not only expedites the diagnostic process but also increases accuracy, leading to better outcomes for individuals.
Furthermore, collaborative platforms are gaining traction, allowing healthcare providers to share insights and best practices. These networks foster a sense of community and cooperation, ultimately enhancing the patient experience by creating a more informed and responsive treatment environment.
Lastly, personalized medicine is reshaping how conditions are treated. By tailoring therapies to individual genetic profiles, practitioners can develop targeted strategies that optimize results. This precision approach reflects a deeper understanding of patient needs, paving the way for more effective interventions.